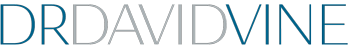
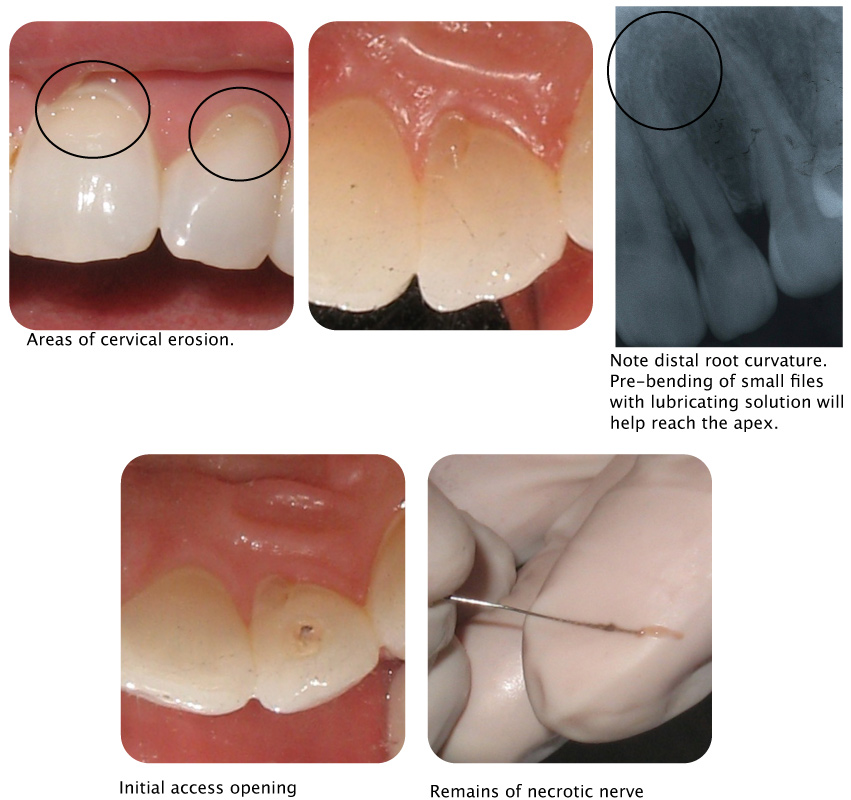
This 30 year old female presented to my office with signs and symptoms of nerve deterioration from the upper left lateral incisor. This tooth is sensitive to percussion and shows no response to an electric pulp test. There doesn’t appear to be occlusal trauma and no other trauma that the patient can recall. There are no restorations on this tooth, no signs of decay ( a small lingual discolored area of tooth structure is evident but doesn’t appear to be carious ) and no root or peri-apical radiolucencies. It was agreed to initiate endodontic therapy. Initial entrance into the recessed canal system was performed without the need for anesthesia. Necrotic tissue along with an oder was evident. Local anesthesia was then administered ( topical plus septicaine ) to make the patient comfortable prior to placing instruments into the apical area. The working length was measured with a apex locater and verfied with a radiograph ( note the distal apical curve ) . The canal system was then instrumented with hand and rotary files ( using EDTA as a lubricant ) and irrigated with antiseptic solutions. Since the patient was going to travel by air in a few days, in order to prevent the possible effect of pressure, a temporary material ( Cavit G ) was placed over a medicated cotton pledget.
Concerning the etiology ( cause ), it is always nice to know why this occurred. What caused this degree of nerve damage , and why on this particular tooth ? In order to at least understand the possibilities, one must go back to the study of anatomy, physiology and biochemistry. Analyzing nerve damage at this level can be quite complex and without more sophisticated tests results may not be apparent. The patient had a habit of grinding her teeth but this did not seem to affect this particular tooth. She was also utilizing Sensodyne ProNamel.