… and other clinical discussion
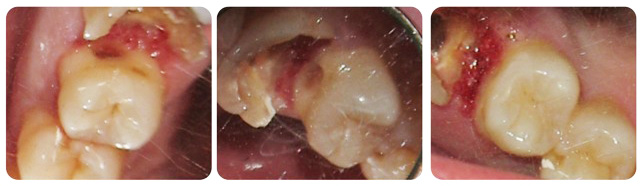
This patient, a physician, came to me with an asymptomatic upper right first molar. Following administration of local anesthesia (topical plus xylocaine with 1:50,000 epinephrine) the defective restoration was removed. Extensive bleeding came from the mesial subgingival area. Additional anesthesia with epinephrine was infiltrated in the area for hemostasis. Once the canals were located endodontic therapy was performed. There are several issues here. I am not an endodontist though I perform many endodontic procedures. I don’t utilize the state of the art microscope that many endodontists utilize, I do use 4.5 magnification lenses. I’ve made efforts over many years to go with my patients when they needed endodontic treatment and have read many books on the subject. Regardless, doing root canal therapy on a molar is not easy. I am generally dissapointed with the radiographic appearance of the gutta percha obturation on the smaller canals. I remember speaking with an endodontic instructor years ago who told me it’s not what you put into the canal that’s important but what you take out of the canal. So, I clean these canals very thoroughly and though the obturation my not appear perfect on the radiograph, most times these teeth remain asymptomatic. Over the years when I see new patients I very often see obturations that are less than ideal with teeth that seem to be doing fine.
The other issue here is that of the biological width. Since the mesial decay extended to bone, is it absolutely necessary to perform crown lengthening ? In an ideal world I guess the answer would be yes. But then you would have to subject the patient to the time and expense of going to a periodontist (unless you as a general dentist perform this procedure, but it’s still surgery). I don’t know that utilizing this procedure would be absolutely necessary.
Following endodontic therapy a carbon fiber post/core would be placed followed by a crown restoration.
While preparing this molar for endodontic therapy, I noticed decay on the distal adjacent surface of the second bicuspid. Now is the time to perform conservative therapy on this tooth (once endodontics is completed on the molar along with a final restoration, access to this area of decay is greatly compromised). The decay was removed and a flowable composite material was utilized to restore this tooth.