September 4, 2014
Diagnosis:
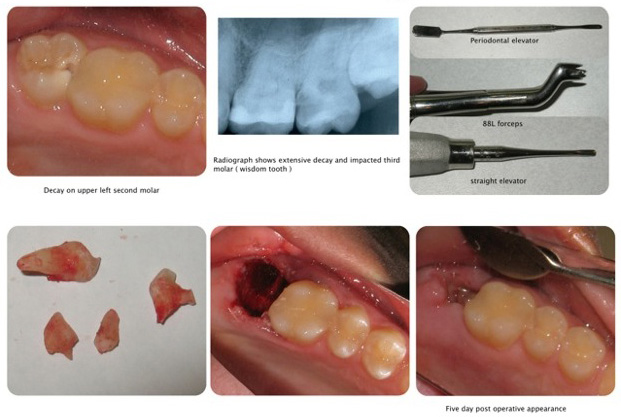
This very nice patient presented with deep decay on an upper left second molar. She was in pain.
Treatment considerations:
Basically this tooth was salvageable however it would require endodontic therapy and a post/core and crown restoration.
The third molar was impacted. It would be nice to simply extract the second molar and have he third molar move into its place however I was told that this generally doesn’t occur naturally and would most likely have to be “pulled” into place orthodontically.
The other factor that is always relevant in private practice is the cost of therapy.
This patient said she could not afford dental therapy. When I questioned her a bit more she said that she could pay about $ 50.00 a month. So I suggested extracting the tooth and since her mother in law had been a patient here for a long time I would reduce the fee for the extraction to $350.00. She agreed.
About extractions:
There are simple extractions and then there are more complex extractions. As a general dentist (1972 graduate of the Baltimore College of Dental Surgery) I have learned how to perform most extractions by reading books and by accompanying my patient to surgeons that showed me how to do the more difficult extractions. This took time and effort however it was like planning for the future in regards to being able to avoid having to refer a patient out and also bringing in revenue that is necessary in private practice.
I wish I could always predict how difficult an extraction might be. I know that with endodontically treated teeth that have deteriorated there is a good chance that the roots have ankylosed to the bone and therefore would become more difficult to extract. On this particular non-endodontic tooth I did not anticipate a problem. Working with two experienced dental assistants always helps .
I administered local anesthesia (topical plus septicaine). I utilized a periodontal elevator to gently detach the gingival tissue from the tooth. I then utilized a straight elevator to torque the tooth and get some movement. I discovered very little movement. I then utilized a forceps to engage the sub-gingival tooth structure and slowly attempt to mobilize the tooth. The tooth was not loosening and the crown eventually disintegrated in pieces due to the infiltration of deep decay. I was now left with rather bloody and difficult to access decayed broken tooth. When necessary in order to obtain better vision and create hemostasis I will inject xylocaine with 1:50,000 epinephrine.
At this point it was necessary to reflect a buccal flap. Once this was performed I utilized a diamond bur to remove buccal bone (osseous tissue) so that I could see and separate the two buccal roots. Again, access was difficult but having two experienced dental assistants helped a lot. Once the two buccal roots were accessed and separated I again utilized a straight elevator to torque them out. The roots fractured again necessitating further osseous resection. Finally I was able to torque them out. The next step was to extract the palatal root. With the buccal roots removed my access to this last root was made easier and this root was gently removed.
Wow, not an easy extraction (It took over two hours, maybe a specialist could have done this is less time). Which brings up another factor. If you’re going to accept dental insurance or work under a government or third party payment plan you are subject to restrictions on fees that don’t take into account the complexity or difficulty encountered. You who have paid the price to develop expert skills and help people and now are being regulated or evaluated to some extent by less educated bureaucrats or clerks. Try to avoid this trap if you can. There’s value to what you do.
Getting back to our patient, once all the tooth structure was removed the patient was given two Advil analgesics and was told to bite down on moisten gauze. After a few minutes of compressing the flap with moisten gauze it was determined that placing sutures was not necessary. The disadvantage of placing sutures is the time required and the fact that they accumulate plaque and bacteria. When indicated, they serve a purpose. We reviewed and dispensed post operative directions, narcotic analgesics (Vicodin ES), extra gauze and an ice pack. I always call the patient that night to see how they’re doing.